Staying hydrated is especially important for protecting your heart health.
Whether you’re going for a run, sitting on your couch recovering from a bad flu, or sitting out in the hot sun, you’ve probably heard the same advice: Get plenty of fluids.
Drinking enough fluids prevents you from getting dehydrated. Dehydration is more than just feeling thirsty – it’s when you lose or use more fluid than you take in, and your body doesn’t have the water it needs to function correctly.
Staying hydrated is critical for staying healthy, and it’s especially important for maintaining a healthy heart.
Also read: American Heart Month: Heart Health FAQs
Here are 6 things to know about the effects of dehydration on your heart and how you can stay hydrated:
1. Dehydration Affects How Your Heart Pumps.
When you’re hydrated, it’s easier for your heart to pump blood throughout your body. But when you’re not well-hydrated, your heart has to work harder. Dehydration makes your blood thicker, which causes difficulty with circulation. It also makes your heart beat faster, which increases heart rate. In more severe cases, dehydration can lead to dangerously high or low spikes in blood pressure.
The benefits of hydration for your health might not be just short-term. Recent research shows that consistently staying hydrated could potentially reduce your risk for heart failure in the future.
2. Staying Hydrated Can Be Tricky if You Have Heart Failure.
If you have severe or advanced heart failure, you have to walk a fine line when it comes to hydration.
Reducing fluid intake is one way that people manage heart failure. Heart failure can cause fluid to build up in your body, which can cause symptoms like shortness of breath or swelling in your legs or stomach. Limiting fluids can decrease your risk of a fluid buildup.
However, if you restrict fluids too much, you can become dehydrated.
Guidelines suggest limiting fluids to 50 oz. a day, but that may or may not be enough for you. Everyone has different needs, so it’s key to talk to your provider to determine the right amount of water so that you can keep managing heart failure without sacrificing hydration.
Read on Duly Health and Care: The Benefits of Drinking Water Go Beyond Quenching Thirst
3. Not Everyone Needs the Same Amount of Water.
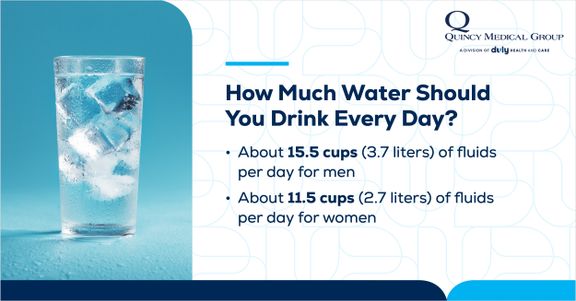
While there isn’t a magical number, there are some general recommendations for water intake.
Some people need more water than others. Your needs might be higher if you are:
- Living with a chronic condition like diabetes or heart disease
- Taking a medication that acts as a diuretic (which makes you urinate more often and lose more fluid)
- Frequently spending time outdoors in the heat or sun
- Over age 50
- Obese or overweight
- Pregnant or breastfeeding
- Sick with symptoms like fever, vomiting, or diarrhea
- Traveling to a new climate
4. Up Your Water Game During Physical Activity.
You lose water through sweat, which is why you need extra water during physical activity to stay hydrated. The amount depends on several factors, like the type and intensity of exercise, the climate you’re exercising in, and what you’re wearing. Also, if you sweat a lot, you might need more water than someone doing the same activity who doesn’t sweat as much.
When you’re physically active outdoors, pay extra attention to staying hydrated. About an hour or two beforehand, drink at least 16 to 20 ounces of fluid. While you’re outside, drink about 6 to 12 ounces every 10 to 15 minutes. Keep on drinking after you’re done – at least another 16 to 24 ounces to make up for the water lost.
Also read: Five Tips for Proper Hydration
5. Drinking Water Isn’t the Only Way to Hydrate.
If the thought of drinking 10+ cups of water a day stresses you out, don’t worry – there are plenty of ways to hydrate without gulping down water. The recommended amount of daily fluid intake also includes water from foods or other beverages.
Some of the most hydrating foods include:
- Asparagus
- Bell peppers
- Berries
- Celery
- Cucumbers
- Lettuce
- Oranges
- Soup
- Tomatoes
- Watermelon
- Zucchini
When it comes to beverages, herbal teas, juice, and milk are mostly made of water. And if you’re a caffeine or carbonation drinker, rejoice – coffee and soda can both contribute to your daily fluid intake. However, be careful about which drinks you choose. Many sodas, sports drinks, and coffee drinks have lots of added sugar and calories.
6. Dehydration Can Be a Medical Emergency.
One of the first signs of dehydration is feeling thirsty. If dehydration is mild or moderate, you might also notice a dry mouth and tongue, headache, tiredness, or darker colored urine. These can be symptoms of mild and moderate dehydration, which usually doesn’t require medical care. Drinking water is the quickest way to rehydrate.
However, there are times when severe dehydration is an emergency that needs medical care right away. Get emergency care immediately if you have:
- Confusion, slurred speech, or hallucinations
- Dizziness, fainting, or loss of consciousness
- A fever of 103°F or higher
- A lack of sweating
- Muscle twitching
- A rapid pulse
- Red, dry, and hot skin
- Seizures
Staying hydrated is essential for your heart health, but there are many other ways to show your heart some love. Talk to your provider about the best ways to keep your heart healthy – and in the meantime, get in those fluids.
Want to learn more ways to keep your heart healthy? Schedule an appointment with a Quincy Medical Group primary care provider. For help managing an existing heart condition, make an appointment with a Quincy Medical Group cardiology expert.
Health Topics:








